Cancer mutation gains ground as test for immunotherapy drugs
September 09, 2017
Scientists are stepping up the hunt for better diagnostic tests to predict if cancer patients will benefit from costly modern immunotherapy drugs, which are transforming cancer care but remain a hit-and-miss affair.
Research presented at Europe’s biggest oncology congress in Madrid adds to evidence that patients with an above average number of genetic mutations in their tumors have a better chance of responding to the new treatments, and drugmakers are racing to confirm the idea.tumors have a better chance of responding to the new treatments, and drugmakers are racing to confirm the idea.
Immuno-oncology (I-O) drugs such as Merck & Co’s Keytruda and Bristol-Myers Squibb’s Opdivo, which help the immune system attack tumors, can have dramatic effects and yet only around 20 to 30 percent of patients show a lasting improvement.
Analyzing the number of mutations within a tumor makes sense: the more there are, the more the patient’s killer T-cells - whose action is enhanced by I-O medicines - will recognize the cancer as foreign to the body and therefore attack it.
Such analysis to measure what is known as tumor mutation burden (TMB) should lead to better targeting of medicines that have a typical list price of near $150,000 a year. It could also mean subgroups of patients with tumors where immunotherapy is not normally considered, like breast cancer, might get them.tumor mutation burden (TMB) should lead to better targeting of medicines that have a typical list price of near $150,000 a year. It could also mean subgroups of patients with tumors where immunotherapy is not normally considered, like breast cancer, might get them.
Progress is being made in applying the idea in practice, with Roche - a global leader in diagnostics as well as the top maker of cancer drugs - demonstrating for the first time on Friday that a blood-based test for TMB can accurately measure mutations.
The Swiss group, which developed the test with majority-owned Foundation Medicine, presented data linking high TMB to improved results for patients in two lung cancer trials at the European Society for Medical Oncology (ESMO) congress.
Doctors welcomed the results but said more evidence was still needed.
Roche is not alone in seeking to use TMB as a new measurable biological signature, or biomarker, with which to personalize I-O treatment.
Bristol-Myers also has a deal with Foundation Medicine and the U.S. drugmaker’s head of medical oncology development, Fouad Namouni, sees TMB testing emerging as a powerful new tool.
“We are moving the needle pretty fast and I am sure in the next few years patients will be tested for TMB and will be treated on the basis of that,” he said. “We are looking at TMB in every major study we are doing.”
BLUNT INSTRUMENT
At present, the one established way of selecting patients for drugs like Keytruda, Opdivo and Roche’s Tecentriq is to test for a protein called PDL-1 in their tumors.
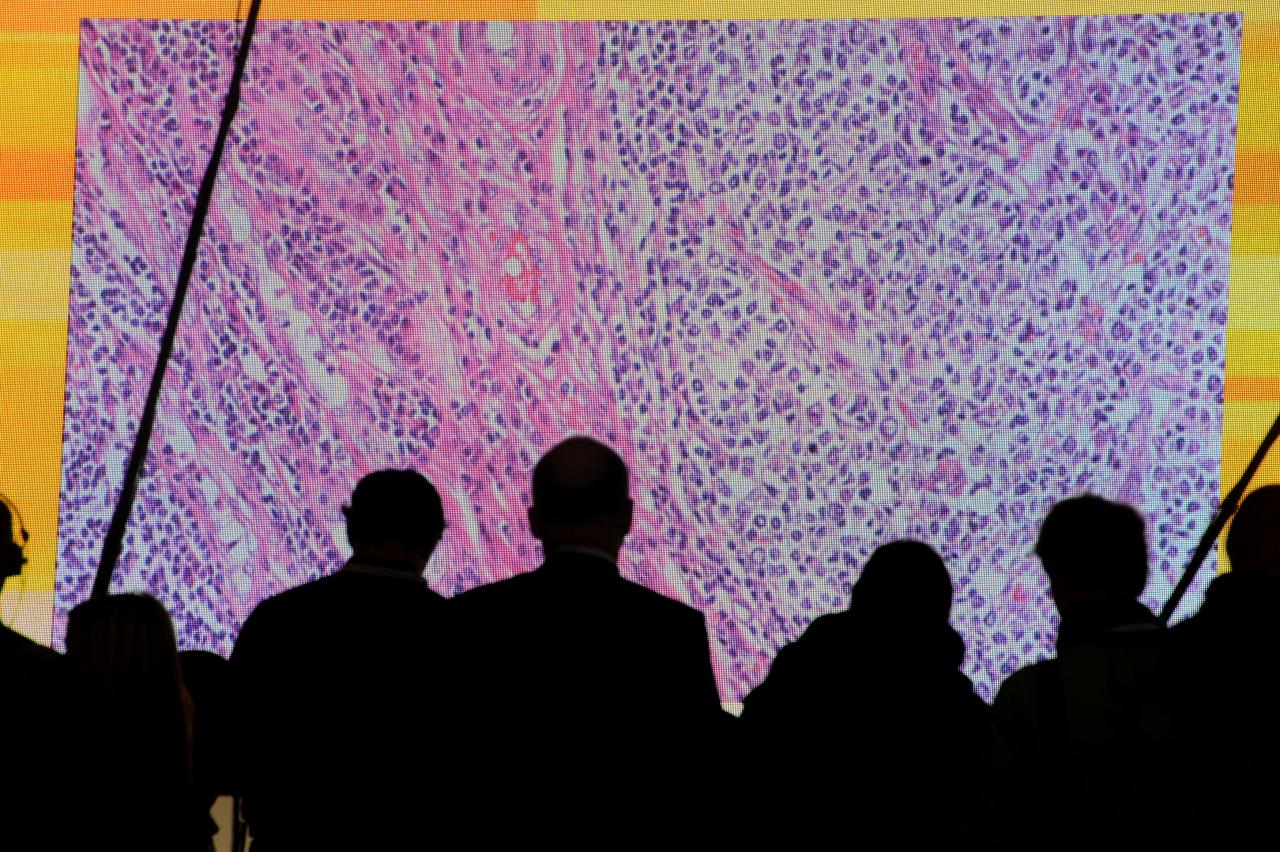
But that involves scientists looking at cells through a microscope and making a qualitative assessment based on their judgment. Clinical trials suggest it is a relatively blunt instrument for predicting a patient’s response to a given treatment.
A quantitative blood test is a quicker and simpler option, doing away with the need to take a tissue biopsy, which until now has been the only reliable way to measure TMB levels.
Thomas Buechele, Roche’s head of global medical affairs in haematology and oncology, believes this may eventually lead to patients with a high level of mutations needing only one I-O drug while those with lower levels get a combination therapy.
Oncologists in Madrid said prospective clinical trials still needed to prove the tests could accurately predict responses, rather than just correlating to outcomes after the event.
“It’s early days but this is clearly one way to go to address the shortcomings of PD-L1 testing,” said Stefan Zimmermann, senior oncologist at Switzerland’s HFR Fribourg-Cantonal Hospital.
While a blood-based test would be a boon for convenience and affordability, the genetic detail it provides is inevitably less than with the more costly and time-consuming process of taking a tissue sample and sequencing tumor DNA.
“It’s clear it is a biomarker – the only question is how good a biomarker is it?” said Jeffrey Weber, professor of medicine at NYU School of Medicine.
Nonetheless, the more researchers learn about the complexities of cancer immunotherapy, the more it becomes apparent that treatment needs to be customized according to the different profiles of individual patients.
One sign of that came last May when Keytruda became the first cancer treatment ever to win US approval based on whether a patient’s tumor carried a specific genetic glitch, irrespective of its location.
Solange Peters of the Centre Hospitalier Universitaire Vaudois in Lausanne said an important issue would be establishing that TMB testing didn’t miss patients who might benefit.
“What we don’t want is to have a test with a very low negative predictive value and thereby prevent patients getting immunotherapy because the biomarker wasn’t good enough.”











