'Rare-blood cancer progression may be reduced to 74% with immune cells'
Researchers will now be following participants to determine long-term effects and impacts on quality of life
June 05, 2023
New trial results presented Monday revealed treatment in which genetically modified human immune cells could decrease the risk of disease progression by 74% in people with rare-found blood cancer, reported AFP.
Ciltacabtagene autoleucel — also known by its trade name Carvykti — was tested on 419 patients with multiple myeloma, whose disease was not responsive to the current frontline drug lenalidomide, a chemotherapy medicine.
Oncologist Oreofe Odejide at the American Society of Clinical Oncology’s annual meeting, said: "Lenalidomide has become a foundation of care for people with myeloma, but as its use has expanded, so has the number of patients whose disease will no longer respond to the treatment."
Ciltacabtagene autoleucel "delivers remarkably effective outcomes compared to patients’ current options" and "can be used safely earlier in the treatment phase," added Odejide, an expert who was not part of the research.
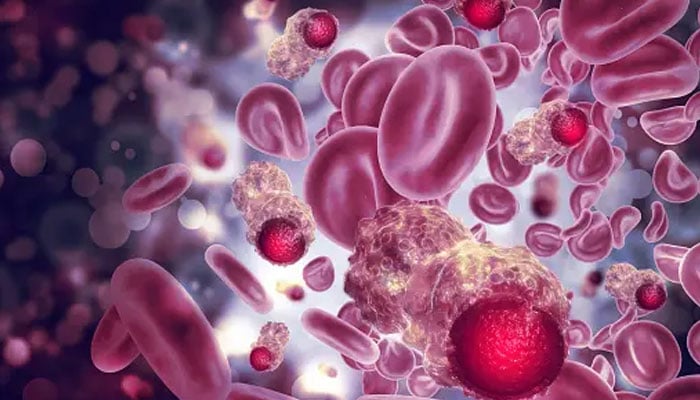
Multiple myeloma affects a type of white blood cells called plasma cells and can cause cascading harm to the bones, kidneys, and immune health.
According to the Cleveland Clinic, it affects seven people out of 100,000 every year with 100,000 people impacted in the US. There is currently no cure to treat the disease, but the progression can be stopped for a long time.
The risk of the disease increases with age, with men more likely to be affected than women, and Black people at higher risk than other races.
However, not everyone needs to be treated immediately and it can be monitored if it is growing slowly.
In the new clinical trial, half the patients were randomly assigned ciltacabtagene autoleucel, while the other half received a cocktail of drugs that represents the current standard of care, including chemotherapy and steroids.
"After a median follow-up of 16 months, the researchers found that ciltacabtagene autoleucel reduced the risk of disease progression by 74%, compared with the standard-of-care treatments," a press statement said.
Ciltacabtagene autoleucel is a type of chimeric antigen receptor (CAR) T-cell therapy, a newer form of treatment.
CAR T-cell therapy involves removing the patient’s disease-fighting T cells, and genetically engineering them in a lab so they have specific proteins known as receptors that, once returned to the body, will seek out and destroy cancer cells.
Nearly all the patients in both groups experienced severe to life-threatening adverse events, including infections and low blood cell counts.
Three-quarters of patients on ciltacabtagene autoleucel developed Cytokine release syndrome, in which the immune system is sent into overdrive. It can affect multiple organs and cause death.
Around 5% of patients on ciltacabtagene autoleucel developed immune effector cell-associated neurotoxicity syndrome (ICANS), which affects a person's nervous system.
In the next step, the researchers said they will be following the participants to determine long-term effects and impacts on quality of life.